Montgomery’s situation is only one of many across California, and the nation writ large, in which an individual’s health is in jeopardy as a result of the machinations of a little-known species of health care corporation: pharmacy benefit managers (PBMs).
Ostensibly, as their lobbyists contend, the role of PBMs is to bargain with drug manufacturers for discounts and rebates, then furnish the drugs to insurance plans and pharmacies while passing on the negotiated savings — and taking a cut for themselves. PBMs also determine an insurance plan’s “formulary,” i.e. the medications made available to people on a certain plan. The reality is that PBMs, far from mitigating drug costs, leverage their middleman position to dictate the price and availability of prescription medicines, extracting fees and engineering transactions to their advantage. At the end of the chain, adverse financial and health effects are inflicted on everyday people.
…
California has long been notable for its comparatively lax regulatory stance towards PBMs — a gap that state lawmakers had planned to address when, in late August, they passed Senate Bill 966. The bill was coauthored by Democratic State Senators Scott Wiener and Aisha Wahab and backed by a coalition of professional associations and patient rights advocates, including the California Pharmacists Association, the National Community Pharmacists Association and Unite for Safe Medications. SB 966 would have instituted the first medical licensing requirements on PBM operations in the state and bolstered transparency and accountability measures. Passed in the State Senate with resounding bipartisan assent, it then went to the desk of Gov. Gavin Newsom — who, just as advocates had feared, vetoed it.
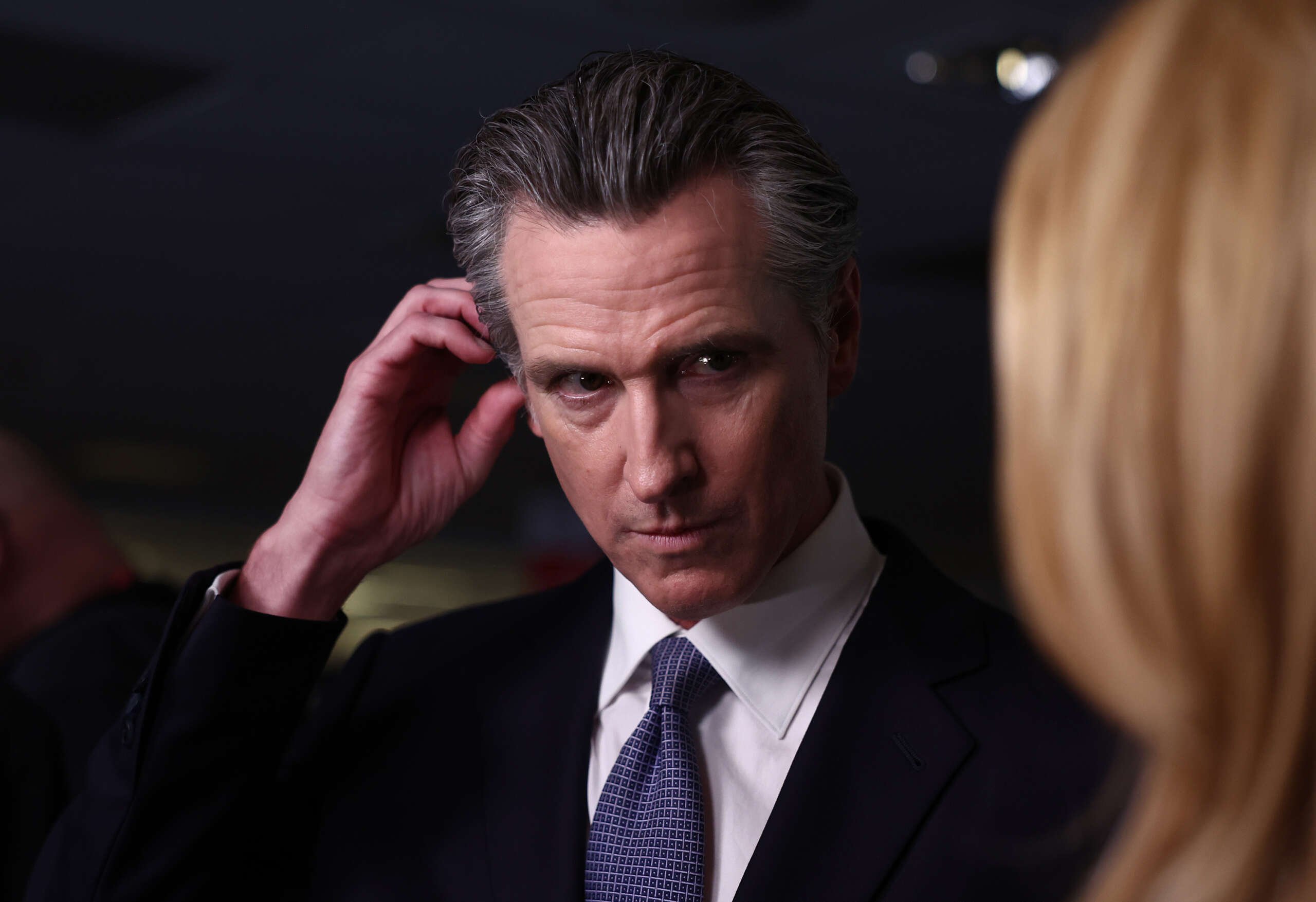
As a pharmacist, this makes my blood boil. Fuck that turd.